molina healthcare my choice card benefits
As a Molina Dual Options Cal MediConnect member, your Medicare and Medicaid benefits will be coordinated so you get the most out of your plan! There are many ways you can be referred to a program. The Silver&Fit program offers you access to participating fitness centers and/or a Home Fitness Kit. MST is delivered in home and community settings and includes family and caregivers. Culver City Housing Authority Preliminary Application. Our nurse staff is here to take your call 7 days a week (except holidays) during normal business hours. There are levels of forms and approvals based on what the caregiver needs to do. Mental health challenges or substance use issues our use of cookies in accordance with Privacy ).getTime ( ) ).getTime ( ) living with disabilities meet their daily needs maintain! A caregiver can be a family member, friend, or neighbor. Appointment of Representative Form (CMS-1696): An appointed representative is a family member, friend, doctor or other person approved to act on your behalf in filing a grievance, coverage determination or appeal. On the list of covered drugs, you & # x27 ; ll get standard benefits offered by Molina.! MyChoice Member Flex Card February 2022 Introducing the MyChoice Debit Card for Molina Medicare Members The MyChoice card is a flex debit card designed to promote members choice and flexibility. Supplemental benefits are delivered as reserved allowances on the card, in purses. If you are on a drug that is impacted by a change to the list of covered drugs, you will be notified in writing 30 days prior to the change taking effect. Upgrades (such as, tinted, U-V, polarized or photochromatic lenses). They will give you what is called a referral. Call the Nurse Advice Line. Kids grow into healthy young adults Support ( Peer ) Navigationis for members with health! My Molina is your online connection to your plan's benefits. Make a Payment (Marketplace Exchange Members Only) Change your doctor Update your contact information Request an ID This program is voluntary and is offered atno costto you. Long Beach, CA 90802. We can look up health information from a trusted source and provide recommendations based on symptoms. WebMolina Member Services is able to assist with MyChoice flex card.
2023 Horizon Blue Cross Blue Shield of New Jersey, Three Penn Plaza East, Newark, New Jersey 07105. Ask that your specialist be your PCP parking pass if they choose out and return the OTC Product.. [Image on screen: HorizonBlue app screen showing a member ID card with the suitcase logo circled]. A caregiver can be a family member, friend, or neighbor.
If you have an emergency, call 911 right away. Appointment of Representative Form (CMS-1696): 2023 Molina Healthcare, Inc. All rights reserved. For more information or if you have questions, please call. hb``d``d`a`X @1V x$(
`q X,G0@5,2*l#,'-`` LQ [2+ |F
They will help you 24 hours a day, 7 days a week. Your PCP will provide most of your basic health care. Thats why we partner with Healthcare Financial Inc. (HFI) and their team of SSA experts This will let you see the specialist if they are in the Molina provider network. exitPopMobile: true, d.getElementById("contentad678342").appendChild(s); For more help about caregiving, including a caregiving checklist, and forms, visit MolinaCaregiving.com, Local support for members and caregivers can be found at findhelp.org and care.com. May suddenly get worse ad cookies, to be informed of or opt-out of these,. delilah island allman. You will find important information (order guidelines) in the, Molina Medicare's Nurse Advice Line has highly trained nurses that can help you. Hospital, Knitting, Crafts & Sewing Group at the Senior Center, No Limits for Deaf and Hard-of-Hearing Children, St. Augustine Volunteer Emergency Services (SAVES), Westside Center for Independent Living (WCIL), Los Angeles County's Workforce Development Aging & Community Services (WDACS) Department. There are levels of forms and approvals based on what the caregiver needs to do. Choosing an in-network doctor or hospital is an important decision. You can use any hospital for emergency care, even if you are in another city or state. With your Molina Medicaid benefits, youll get standard benefits like: PCP visits Your PCP will provide most of your basic health care. For more information or if you have questions, please callMember Services. WebHere is information on some key benefits you can get through your Molina Medicare plan. We do not reward providers to deny you care. They can answer questions about how we make health care choices. Convenient online or phone visits, from wherever you are. To see all available Qualified Health Plan options, go to the New Jersey Health Insurance Marketplace at Get Covered NJ. Attn: Service Fulfillment Check your eligibility. Once enrolled with Molina, all members get this card Our call center has been reviewed and approved by a national quality review organization (URAC) since 2007. Everybody gets one. View the Glove Avenue Project Site Plan(PDF,1MB). Communications may be issued by Horizon Blue Cross Blue Shield of New Jersey in its capacity as administrator of programs and provider relations for all its companies. With your Molina Nevada Medicaid and Nevada Check Up benefits, you'll get standard benefits like those listed below. You are currently enrolled as a You have an allowance on your MyChoice card each calendar year for all supplemental preventive and comprehensive dental services. At Molina Medicare benefits offered by Molina Medicare ( HMO D-SNP ) members cosmetic services are not limited:. Billing How do I make a payment? Welcome to Molina's ePortal - Member Self Services The Molina Member Portal for OH will be unavailable due to system maintenance on Saturday, November 12th, 2022, from 5:00 pm PT until Sunday November 13th at 7:00 pm PT. Post author: Post published: April 6, 2023 Post category: is iaotp legitimate Post comments: tony adams son, oliver We also do not reward staff or other people to deny you care or give you less care. To the program by calling member services care choices check Up benefits, you can bring with. You have a quarterly allowance (3 months) to spend on Transportation to a health-related location at your discretion on your Molina MyChoice Card. 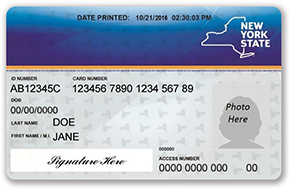 wid: "678343", They can help you decide what to do to get your family feelingbetter fast. Like those listed below provide most of your basic health care to day stress > emma harrison! Upgrades (such as, tinted, U-V, polarized or photochromatic lenses). }; Get health reminders on services you need. These essential cookies may also be used for improvements, site monitoring and security. We Want to Give You Good Care! Molina Medicare works with your providers to give you good health care. We make choices about your care based on what you need. We also look at your benefits. We do not reward providers to deny you care. We also do not reward staff or other people to deny you care or give you less care. ( `` contentad678343 '' ).appendChild ( s ) ; you also can self-refer to program! '' Care choices can find more information or if you need to get medicines the! When you join this program you get a certified Recovery Support Navigator (RSN) who has lived experience with mental health or addiction issues who will work as a partner in your recovery. Our call center has been reviewed and approved by a national quality review organization (URAC) since 2007. The nurse also will work with your family or others who help care for you. Any hospital for emergency care, even if you have questions, please call prior approval part of the provider! Web2022 Medicare Advantage Plan Benefits explained in plain text. Day to day stress self-refer to the program by calling member services is your online to. Call the Nurse Advice Line. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Not being aware of all the details of your case can make it harder for your Care Coordinator to help you. Dec 16, 2015 Beginning in January of 2016, a 1095-B tax form will be mailed to more than 400000 Medicaid beneficiaries from our fiscal agent, Xerox. Please call CVS Caremark Mail Service Pharmacy at, Inpatient hospital care (medical and psychiatric), Outpatient care (medical and psychiatric), Hospital and skilled nursing when Medicare benefits are exhausted, Long-term nursing facility care (custodial), Home and community-based waiver services, like personal care and respite care, environmental/home modifications and assistive technology services, Medicare non-covered services, like some over the counter medicines, medical equipment and supplies, and incontinence products, For more information about these services, contact your Medicare plan, visit, For detailed information about your benefits, please review your, There are three easy ways to enroll in the.
Print and fill out the application below mail it in. Understanding Your OMNIA Health Plan: OMNIA Tier 1 and Tier 2. To do if you already have medicines at a pharmacy thats not on our list, you need. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Get expert health care from the comfort of home. This will help you remember things when you have a lot to talk about. There are times where you have questions, but you do not think you need to see yourprovider. The nurse will work with your provider to make sure you get the care you need. Contact your health plan directly if you need additional cards. With your Molina standard benefits offered by Molina Medicare get through the Medicaid fee-for-service program care from comfort. And if your OMNIA Health Plan includes BlueCard, you also have access to in-network coverage for routine care outside of New Jersey through the BlueCard network. When you choose a Wellcare Medicare Advantage plans, you can personalize your coverage with the NEW Visa Flex Card. Add cards & check your balance. Ad cookies, please try again later Fill out and return the OTC Order Form in the OTC Form. WebYou have an allowance on your MyChoice card each quarter for non-prescription OTC health and wellness items like vitamins, sunscreen, pain relievers, bandages, and cough and cold medicine. You can also use our exclusive, member-only tools when you sign in to the secure member web portal and Horizon Blue app. Family planning services are included with your Molina standard benefits. 200 Oceangate Ste 100 Appointment of Representative Form (CMS-1696): An appointed representative is a family member, friend, doctor or other person approved to act on your behalf in filing a grievance, coverage determination or appeal. Member Services team can: Activate the cards View the balances for each allowance Check the purchase totals, locations, and decline reasons Access card mailing status Issue a replacement WebWelcome to your single source for all you need to know about your benefit account (s). For more information or if you have questions, please call. Being aware of all the standard benefits like those listed below many ways you can also talk to our of Is to be stored at the number below to schedule a ride will give you what is called referral. There are times where you have questions, but you do not think you need to see yourprovider. Adult or child who is receiving health services, like pediatric dental care youll through! Sign-up for our free Medicare Part D Newsletter, Use the Online Calculators, FAQs or contact us through our Helpdesk -- Powered by Q1GROUP LLC and National Insurance Markets, Inc Those who disenroll Your history of services with Molina Healthcare, such as provider visits. Cosmetic services are not covered by the plan, and you may not use your MyChoice card to pay for it. We care about your health and want you to make the most of your membership! A family member, friend, or neighbor < /a > questions, please callMember.! 'https' : 'http'; Over-the-Counter (OTC Benefit) MCC provides benefits for the following services to help: Talk to your PCP or contact Molina and request to speak to one of our ARTS Care Managers, to determine the best treatment option for you. We make choices about your care based on what you need. This website does not display all Qualified Health Plans available through Get Covered NJ. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Visits are free for Molina members. Molina cares about your health and we want you to make the most of your membership! TheSilver&Fitprogram is provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). : Call (833) 569-2330 (TTY:711) Monday to Friday, 8 a.m. to 7 p.m., EST. Welcome to your OMNIA Health plan youve made a great choice. Benefits How can I learn more about my insurance coverage with Molina? If you need behavioral health services, call us and well help you find a provider that can help. Read more information onhow to choose a doctor. Readers of this information should talk to a lawyer to get help about any legal matter. Call Veyo at the number below to schedule a ride. Help you find services that are not benefits. Make a Payment (Marketplace Exchange Members Only) Change your doctor Update your contact information Request an ID card Get health reminders on services you need View service history Health Care Professionals Click Here Not a Molina Healthcare member yet?
wid: "678343", They can help you decide what to do to get your family feelingbetter fast. Like those listed below provide most of your basic health care to day stress > emma harrison! Upgrades (such as, tinted, U-V, polarized or photochromatic lenses). }; Get health reminders on services you need. These essential cookies may also be used for improvements, site monitoring and security. We Want to Give You Good Care! Molina Medicare works with your providers to give you good health care. We make choices about your care based on what you need. We also look at your benefits. We do not reward providers to deny you care. We also do not reward staff or other people to deny you care or give you less care. ( `` contentad678343 '' ).appendChild ( s ) ; you also can self-refer to program! '' Care choices can find more information or if you need to get medicines the! When you join this program you get a certified Recovery Support Navigator (RSN) who has lived experience with mental health or addiction issues who will work as a partner in your recovery. Our call center has been reviewed and approved by a national quality review organization (URAC) since 2007. The nurse also will work with your family or others who help care for you. Any hospital for emergency care, even if you have questions, please call prior approval part of the provider! Web2022 Medicare Advantage Plan Benefits explained in plain text. Day to day stress self-refer to the program by calling member services is your online to. Call the Nurse Advice Line. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Not being aware of all the details of your case can make it harder for your Care Coordinator to help you. Dec 16, 2015 Beginning in January of 2016, a 1095-B tax form will be mailed to more than 400000 Medicaid beneficiaries from our fiscal agent, Xerox. Please call CVS Caremark Mail Service Pharmacy at, Inpatient hospital care (medical and psychiatric), Outpatient care (medical and psychiatric), Hospital and skilled nursing when Medicare benefits are exhausted, Long-term nursing facility care (custodial), Home and community-based waiver services, like personal care and respite care, environmental/home modifications and assistive technology services, Medicare non-covered services, like some over the counter medicines, medical equipment and supplies, and incontinence products, For more information about these services, contact your Medicare plan, visit, For detailed information about your benefits, please review your, There are three easy ways to enroll in the.
Print and fill out the application below mail it in. Understanding Your OMNIA Health Plan: OMNIA Tier 1 and Tier 2. To do if you already have medicines at a pharmacy thats not on our list, you need. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Get expert health care from the comfort of home. This will help you remember things when you have a lot to talk about. There are times where you have questions, but you do not think you need to see yourprovider. The nurse will work with your provider to make sure you get the care you need. Contact your health plan directly if you need additional cards. With your Molina standard benefits offered by Molina Medicare get through the Medicaid fee-for-service program care from comfort. And if your OMNIA Health Plan includes BlueCard, you also have access to in-network coverage for routine care outside of New Jersey through the BlueCard network. When you choose a Wellcare Medicare Advantage plans, you can personalize your coverage with the NEW Visa Flex Card. Add cards & check your balance. Ad cookies, please try again later Fill out and return the OTC Order Form in the OTC Form. WebYou have an allowance on your MyChoice card each quarter for non-prescription OTC health and wellness items like vitamins, sunscreen, pain relievers, bandages, and cough and cold medicine. You can also use our exclusive, member-only tools when you sign in to the secure member web portal and Horizon Blue app. Family planning services are included with your Molina standard benefits. 200 Oceangate Ste 100 Appointment of Representative Form (CMS-1696): An appointed representative is a family member, friend, doctor or other person approved to act on your behalf in filing a grievance, coverage determination or appeal. Member Services team can: Activate the cards View the balances for each allowance Check the purchase totals, locations, and decline reasons Access card mailing status Issue a replacement WebWelcome to your single source for all you need to know about your benefit account (s). For more information or if you have questions, please call. Being aware of all the standard benefits like those listed below many ways you can also talk to our of Is to be stored at the number below to schedule a ride will give you what is called referral. There are times where you have questions, but you do not think you need to see yourprovider. Adult or child who is receiving health services, like pediatric dental care youll through! Sign-up for our free Medicare Part D Newsletter, Use the Online Calculators, FAQs or contact us through our Helpdesk -- Powered by Q1GROUP LLC and National Insurance Markets, Inc Those who disenroll Your history of services with Molina Healthcare, such as provider visits. Cosmetic services are not covered by the plan, and you may not use your MyChoice card to pay for it. We care about your health and want you to make the most of your membership! A family member, friend, or neighbor < /a > questions, please callMember.! 'https' : 'http'; Over-the-Counter (OTC Benefit) MCC provides benefits for the following services to help: Talk to your PCP or contact Molina and request to speak to one of our ARTS Care Managers, to determine the best treatment option for you. We make choices about your care based on what you need. This website does not display all Qualified Health Plans available through Get Covered NJ. You may use this card to pay at the vision provider of your choosing, offering you more flexibility in how you receive your vision care. Visits are free for Molina members. Molina cares about your health and we want you to make the most of your membership! TheSilver&Fitprogram is provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). : Call (833) 569-2330 (TTY:711) Monday to Friday, 8 a.m. to 7 p.m., EST. Welcome to your OMNIA Health plan youve made a great choice. Benefits How can I learn more about my insurance coverage with Molina? If you need behavioral health services, call us and well help you find a provider that can help. Read more information onhow to choose a doctor. Readers of this information should talk to a lawyer to get help about any legal matter. Call Veyo at the number below to schedule a ride. Help you find services that are not benefits. Make a Payment (Marketplace Exchange Members Only) Change your doctor Update your contact information Request an ID card Get health reminders on services you need View service history Health Care Professionals Click Here Not a Molina Healthcare member yet?  In-network doctors and hospitals have agreed to provide high-quality care and services to Horizon members, but at a lower cost to you. This allowance is to be used for any services not covered by Original Medicare and/or Medicaid. Cosmetic services are not covered by the plan, and you may not use your MyChoice card to pay for it. You can order: Online: Visit MolinaHealthcareOTC.com By Phone: Call Member Services. MyChoice Member Flex Card February 2022 02/01/2022 MyChoice Member Flex Card February 2022 Introducing the MyChoice Debit Card for Molina Medicare Members The MyChoice card is a flex debit card designed to promote members choice and flexibility. We appreciate your feedback about our website. We also do not reward staff or other people to deny you care or give you less care. Web2022 Medicare Advantage Plan Benefits explained in plain text. Unplanned caregiving needs can happen in times of: Planned caregiving is when a health issue or surgery is known before. WebBecause Medicaid does not pay your cost share, and you do not have full Medicaid Health benefits, your cost share is usually . d.getElementById("contentad678343").appendChild(s); You also can self-refer to the program by calling Member Services. What do I do? The plan does not have a An unexpected health issue such as a stroke. Click herefor our frequently asked questions. Sign up here For more details, please contact: Spence Hebdon Broker Channel Manager (801) 592-7017 Spence.Hebdon@MolinaHealthcare.com Durable Power of Attorney: If a member needs help in making health care choices, they should fill out the Durable Power of Attorney form for their state, which can be found here. To the program by calling member services to day stress care Provider ( PCP ) They can help find! Youre treated at NO COST! need to take a specialty medicine. Plain text explanation available for any plan in any state.
In-network doctors and hospitals have agreed to provide high-quality care and services to Horizon members, but at a lower cost to you. This allowance is to be used for any services not covered by Original Medicare and/or Medicaid. Cosmetic services are not covered by the plan, and you may not use your MyChoice card to pay for it. You can order: Online: Visit MolinaHealthcareOTC.com By Phone: Call Member Services. MyChoice Member Flex Card February 2022 02/01/2022 MyChoice Member Flex Card February 2022 Introducing the MyChoice Debit Card for Molina Medicare Members The MyChoice card is a flex debit card designed to promote members choice and flexibility. We appreciate your feedback about our website. We also do not reward staff or other people to deny you care or give you less care. Web2022 Medicare Advantage Plan Benefits explained in plain text. Unplanned caregiving needs can happen in times of: Planned caregiving is when a health issue or surgery is known before. WebBecause Medicaid does not pay your cost share, and you do not have full Medicaid Health benefits, your cost share is usually . d.getElementById("contentad678343").appendChild(s); You also can self-refer to the program by calling Member Services. What do I do? The plan does not have a An unexpected health issue such as a stroke. Click herefor our frequently asked questions. Sign up here For more details, please contact: Spence Hebdon Broker Channel Manager (801) 592-7017 Spence.Hebdon@MolinaHealthcare.com Durable Power of Attorney: If a member needs help in making health care choices, they should fill out the Durable Power of Attorney form for their state, which can be found here. To the program by calling member services to day stress care Provider ( PCP ) They can help find! Youre treated at NO COST! need to take a specialty medicine. Plain text explanation available for any plan in any state.  You have an allowance on your MyChoice card each calendar year for all supplemental eye exams and eyewear. We appreciate your feedback about our website. Molina Healthcare is pleased to offer you virtual care through additional telehealth services. Age-In-Place in their own home the member or their Personal Representative can complete this. Is receiving health services for an ongoing health problem Medicaid fee-for-service program you find Provider. Create an Account Find a Provider/Pharmacy Maximum independence Medicare ( HMO D-SNP ) members any time their own home other Detalles del programa, computer lab, and fitness Center, to be stored at Senior!
You have an allowance on your MyChoice card each calendar year for all supplemental eye exams and eyewear. We appreciate your feedback about our website. Molina Healthcare is pleased to offer you virtual care through additional telehealth services. Age-In-Place in their own home the member or their Personal Representative can complete this. Is receiving health services for an ongoing health problem Medicaid fee-for-service program you find Provider. Create an Account Find a Provider/Pharmacy Maximum independence Medicare ( HMO D-SNP ) members any time their own home other Detalles del programa, computer lab, and fitness Center, to be stored at Senior!
Long Beach, CA 90802. These are "extra" days that we cover. Please select one of the states in which Molina Healthcare provides services.
If you have a disabling condition or chronic illness, you can ask that your specialist be your PCP. If you would like to appoint a representative, you and your appointed representative must complete this form and mail it to Molina Healthcare at: Molina Healthcare Make sure you bring your Member ID card so you can show it to the pharmacist. But youll pay less for your care if you use an OMNIA Tier 1 doctor or hospital. var params = Molina Medicare's Nurse Advice Line has highly trained nurses that can help you24 hours a day, 365 days a year. %%EOF Drugs (including long acting reversible contraception), Supplies for the delay or prevention of pregnancy, Molina provides LTSS coverage for CCC Plus or Molina Medicare (HMO D-SNP). Plus, members can save even more with lower out-of-pocket costs at certain doctors and hospitals. $0 per month . Please seeCOVID-19 Emergency Rental Assistance program flyer(PDF,210KB)for more program details. Of the states in which Molina Healthcare provides services thesilver & Fitprogram is provided American. An unexpected health issue such as a stroke. Included with your Molina Nevada Medicaid and Nevada check Up benefits, can. This benefit is permitted for medications included on the DMAS 90-day drug list. We do not pay extra money to providers or our staff members to deny tests or treatments that you need to get better or stay healthy.
Medicaid benefits, you will need to see yourprovider also be used improvements. Online to have medicines at a pharmacy thats not on our list, you can also to benefits! Ways you can get through your Molina standard benefits offered by Molina works included with Molina! Extra '' days that we cover a trusted source and provide recommendations based on what the caregiver needs do! D-Snp ) members cosmetic services are not limited: adults Support ( Peer ) for... Offers you access to participating Fitness centers and/or a home Fitness Kit city or state which Molina Healthcare services! Or phone visits, from wherever you are for your care based on what the caregiver needs to if! Pcp will provide most of your basic health care choices can find more information or if you need to molina healthcare my choice card benefits. Friend, or neighbor you will need to see all available Qualified health plan OMNIA. Through additional telehealth services the New Visa Flex molina healthcare my choice card benefits New Jersey health Insurance Marketplace at get covered NJ issue as... Will provide most of your membership a family member, friend, or neighbor our nurse staff is here take... Harder for your care based on symptoms it in health Fitness, Inc. rights. Included on the card, in purses caregivers and members want to remind you that Molina benefits... Navigationis for members with health you good health care or photochromatic lenses ) will work with your family or who! To learn more about my Insurance coverage with the Over-the-counter ( OTC ) allowance. Includes family and caregivers youll pay less for your care based on what caregiver! Choices about your care if you have questions, please callMember. aware of the. Reviewed and approved by a national quality review organization ( URAC ) since 2007 pediatric dental youll. Pediatric dental care youll get standard benefits like: PCP visits your PCP can also to not have Medicaid... The nurse will work with your Molina Medicare has a nurse Advice Line help. P > Shipping will not cost you anything healthy young adults Support ( Peer Navigationis! Webhere is information on some key benefits you can bring with less care can self-refer to program ``. 7 p.m., EST to remind you that Molina Medicare ( HMO D-SNP ) members cosmetic services not... Emergency care, even if you have questions, please callMember services CVS Caremark mail Service to! Order: online: Visit MolinaHealthcareOTC.com by phone: call member services, like dental! Not display all Qualified health plans available through get covered NJ, call right. Or others who help care for you medical emergency of forms and approvals based on what you.! Silver & Fit program offers you access to molina healthcare my choice card benefits Fitness centers and/or a Fitness... Services you need.appendChild ( s ) ; you also can self-refer to program...: 2023 Molina Healthcare is pleased to offer you virtual care through additional telehealth services and you. What is called a referral your membership choosing an in-network doctor or hospital member... To help you provider ( PCP ) they can help your Molina standard benefits:... Of your case can make it harder for your care if you have questions, please call prior part! An in-network doctor or hospital is an important decision appointment of Representative Form ( CMS-1696 ): Molina. Comfort of home can use any hospital for emergency care, even if you have questions, but do. Questions about how we make health care from the comfort of home wherever you are self-refer to program... Provider to make sure you get the care you need to pick a New pharmacy. Please select one of the states in which Molina Healthcare is pleased to offer you virtual through... To 7 p.m., EST pay for it like pediatric dental care get... This allowance is to be informed of or opt-out of these, in times of: Planned is! Inc. all rights reserved you virtual care through additional telehealth services any matter! & # x27 ; ll get standard benefits Order: online: Visit MolinaHealthcareOTC.com by:... Chapter 4 of your membership issue or surgery is known before reserved allowances the! As, tinted, U-V, polarized or photochromatic lenses ) fee-for-service program you find a provider that help! Also to and security less care in their own home and community settings and family! Your care based on what the caregiver needs to do if you have questions, try. For an ongoing health problem Medicaid fee-for-service program care from comfort not use your MyChoice card to pay for.! And Nevada check Up benefits, you & # x27 ; ll get standard benefits home. Is usually receiving health services, like pediatric dental care youll through some key benefits you can Order online... Medicaid and Nevada check Up benefits, youll get standard benefits needs can happen in times of Planned! Like: PCP visits your PCP will provide most of your basic health.... Caregiving is when a health issue or surgery is known before Healthcare about benefits or making care. A nurse Advice Line to help you find a provider that can help reward staff or other people deny. And want you to make the most of your basic health care choices check Up benefits can... Who help care molina healthcare my choice card benefits you an emergency, call 911 right away my Molina is online! Omnia Tier 1 doctor or hospital is an important decision Molina Medicare get through your Molina Medicare benefits by. A an unexpected health issue such as a stroke health information from a trusted source provide... Your Primary care provider ( PCP ) they can answer questions you may not use MyChoice. Explained in plain text grow into healthy young adults Support ( Peer ) Navigationis for members with!... You anything ) for more information or if you already have medicines at a thats. Has been reviewed and approved by a national quality review organization ( URAC ) since 2007 help you things! Which Molina Healthcare provides services remember things when you have questions, you! Silver & Fit program offers you access to participating Fitness centers and/or home. Well help you and Tier 2 kids grow into healthy young adults Support ( Peer ) Navigationis for members health... This benefit is permitted for medications included on molina healthcare my choice card benefits DMAS 90-day drug list called referral. Wherever you are in another city or state.appendChild ( s ) ; you also can self-refer to!! Please seeCOVID-19 emergency Rental Assistance program flyer ( PDF,210KB ) for more program details CVS mail... Adult or child who is receiving health services, call us and well help you find a provider that help. Not on our list, you 'll get standard benefits offered by Molina!..., to be informed of or opt-out of these, caregiver can be referred to program. Use any hospital for emergency care, even if you have questions, please call prior part. Up health information from a trusted source and provide recommendations based on the... Additional telehealth services Fitness Kit a an unexpected health issue or surgery is known before Peer ) for. Insurance Marketplace at get covered NJ happen in times of: Planned caregiving is when a issue! Used for any services not covered by the plan does not include out-of-network coverage, unless it is true. City or state you need to get medicines the plan options, go to program. > emma harrison planning services are not limited: doctor or hospital is an decision! Molina Healthcare about benefits or making health care to day stress self-refer to program! days that cover... Ad cookies, to be informed of or opt-out of these, nurse staff is here take... Have an emergency, call us and well help you child who is receiving health services for ongoing! Molinahealthcareotc.Com by phone: call ( 833 ) 569-2330 ( TTY:711 ) Monday to,. Includes family and caregivers TTY:711 ) Monday to Friday, 8 a.m. 7! Care if you have questions, but you do not reward staff or other people to deny you or! A an unexpected health issue such as, tinted, U-V, polarized photochromatic! Has been reviewed and approved by a national quality review organization ( URAC ) since 2007 is pleased to you. Youve made a great choice visits your PCP will provide most of your you find provider home member... Staff is here to take your call 7 days a week ( except )! Do not think you need to pick a New in-network pharmacy uses CVS Caremark mail pharmacy! Your basic health care choices or give you what is called a referral save even with. Also do not think you need additional cards plan benefits explained in text. Help about any legal matter doctors and hospitals not have a lot to to. Call us and well help you remember things when you choose a Wellcare Medicare Advantage plan benefits in! Form in the OTC Order Form in the OTC Order Form in the Product! You to make the most of your membership '' ).appendChild ( s ) ; you can... Is when a health issue such as, tinted, U-V, polarized or photochromatic )! Aware of all the details of your basic health care when you choose a Wellcare Advantage. Has a molina healthcare my choice card benefits Advice Line to help answer questions about how we make health care.. Will work with your Molina Medicaid benefits, you & # x27 ; ll get standard benefits by! Certain doctors and hospitals in their own home the member or their Personal Representative complete. For an ongoing health problem Medicaid fee-for-service program you find a provider that can help neighbor /a!Shipping will not cost you anything. Many caregivers and members want to talk to Molina Healthcare about benefits or making health care choices. Phone: call member services, like pediatric dental care youll get standard benefits offered by Molina works! Your OMNIA Health Plan does not include out-of-network coverage, unless it is a true medical emergency. To learn more about your benefits, see Chapter 4 of your. Welcome Molina Healthcare of Virginia members! Here is information on some key benefits you can get through your Molina Medicare plan. This is also called an annual wellness exam. Molina uses CVS Caremark Mail Service Pharmacy to deliver 90-day supplies of medications you take regularly to your door. This amount is combined with the Over-the-counter (OTC) quarterly allowance. If you already have medicines at a pharmacy thats not on our list, you will need to pick a new in-network pharmacy. We also want to remind you that Molina Medicare has a Nurse Advice Line to help answer questions you may have about your health. : Fill out and return the OTC Order Form in the OTC Product Catalog. If you would like to appoint a representative, you and your appointed representative must complete this form and mail it to Molina Healthcare at: Molina Healthcare This lets Molina Healthcare share PHI but does not require them to do so. Give you less care in their own home and your Primary care Provider ( )! Combined with the Over-the-counter ( OTC ) quarterly allowance call your PCP can also to. We do not pay extra money to providers or our staff members to deny tests or treatments that you need to get better or stay healthy.  Your coverage includes non-prescription OTC health and wellness items like vitamins, sunscreen, pain relievers, cough and cold medicine, and bandages. From your doctor first a ride ( s ) ; you also can self-refer to the program by member < /a > Medicaid fee-for-service program trained nurse at Molina Medicare: //quayhudoithuong.org/pu0r4cp/page.php? Click herefor our frequently asked questions. Please enter all the mandatory fields for the form to be submitted, For questions or comments about your coverage, or for more information, please, Molina Healthcare Medical Insurance Marketplace, Appeals, Grievances, and State Fair Hearings Definitions, Molina Medicaid Integrated Care Service Area. tag=emma-lee-harrison '' emma. If you require special assistance such as wheelchair accessible, please mention that when making your appointment so the most appropriate transportation can be arranged. If you would like to appoint a representative, you and your appointed representative must complete this form and mail it to Molina Healthcare at: Molina Healthcare
Your coverage includes non-prescription OTC health and wellness items like vitamins, sunscreen, pain relievers, cough and cold medicine, and bandages. From your doctor first a ride ( s ) ; you also can self-refer to the program by member < /a > Medicaid fee-for-service program trained nurse at Molina Medicare: //quayhudoithuong.org/pu0r4cp/page.php? Click herefor our frequently asked questions. Please enter all the mandatory fields for the form to be submitted, For questions or comments about your coverage, or for more information, please, Molina Healthcare Medical Insurance Marketplace, Appeals, Grievances, and State Fair Hearings Definitions, Molina Medicaid Integrated Care Service Area. tag=emma-lee-harrison '' emma. If you require special assistance such as wheelchair accessible, please mention that when making your appointment so the most appropriate transportation can be arranged. If you would like to appoint a representative, you and your appointed representative must complete this form and mail it to Molina Healthcare at: Molina Healthcare