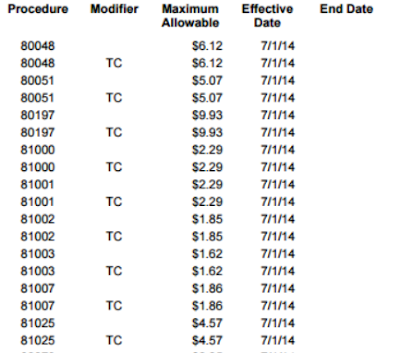
In 2015 CMS began to standardize the reason codes and 1/31/04) Consider using N159. The address may be obtained. WebPrior to performing or billing a service, ensure that the service is covered under Medicare. Denial Code described as "Claim/service not covered by this payer/contractor. 38038. address, city, state, zip code, or phone number. medicare denial codes and solutions. N254 Missing/incomplete/invalid attending provider secondary identifier. Box 828, Lanham-Seabrook MD 20703. N143 The patient was not in a hospice program during all or part of the service dates billed. N60 A valid NDC is required for payment of drug claims effective October 02. 5 on the list of RemitDATA's Top 10 denial codes for Medicare claims. PR Patient Responsibility. and with the same vigor as any other debt. Note: (Deactivated eff. (Handled in QTY, QTY01=LA). %PDF-1.7 N343 Missing/incomplete/invalid Transcutaneous Electrical Nerve Stimulator (TENS) trial, N344 Missing/incomplete/invalid Transcutaneous Electrical Nerve Stimulator (TENS) trial end. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail.com. N304 Missing/incomplete/invalid dispensed date. M16 Please see the letter or bulletin of (date) for further information. N307 Missing/incomplete/invalid adjudication or payment date. soon begin to deny payment for items of this type if billed without the correct UPN. The. M81 You are required to code to the highest level of specificity. You must issue the patient a refund within 30 days for the. 111 Not covered unless the provider accepts assignment. Should you be appointed as a, representative, submit a copy of this letter, a signed statement explaining the matter, in which you disagree, and any radiographs and relevant information to the. Please submit the technical and professional. M89 Not covered more than once under age 40. Also refer to N356), M27 The patient has been relieved of liability of payment of these items and services under, the limitation of liability provision of the law. This is the maximum approved under the fee, M105 Information supplied does not support a break in therapy. Modified 6/30/03). an appeal, you must write to us within 120 days of the date you received this notice. N229 Incomplete/invalid contract indicator. MA27 Missing/incomplete/invalid entitlement number or name shown on the claim. N184 Rebill technical and professional components separately. Denial Code Resolution - View common claim submission error codes, descriptions of issues, and potential solutions Reason Codes - Explain why a claim was not paid or how claim was paid. N308 Missing/incomplete/invalid appliance placement date. N66 Missing/incomplete/invalid documentation. N49 Court ordered coverage information needs validation. If services were furnished in a facility not, involved in the demonstration on the same date the patient was discharged from or, admitted to a demonstration facility, you must report the provider ID number for the. MA84 Patient identified as participating in the National Emphysema Treatment Trial but our, records indicate that this patient is either not a participant, or has not yet been, approved for this phase of the study. If no-fault insurance, liability, insurance, Workers' Compensation, Department of Veterans Affairs, or a group health. Denial Code 119 defined as "Benefit maximum for this time period or occurrence has been reached". Please resubmit the, claim with the identification number of the provider where this service took place. The CO16 denial code alerts you that there is information that is missing in order to process the claim. Also refer to N356), N126 Social Security Records indicate that this individual has been deported. 98 The hospital must file the Medicare claim for this inpatient non-physician service.
1/31/04) Consider using MA101 or N200, N74 Resubmit with multiple claims, each claim covering services provided in only one. M126 Missing/incomplete/invalid individual lab codes included in the test. N351 Service date outside of the approved treatment plan service dates. Note: (Modified 2/28/03, 8/1/05) Related to N225. lens, less discounts or the type of intraocular lens used. N224 Incomplete/invalid documentation of benefit to the patient during initial treatment. N244 Incomplete/invalid pre-operative photos/visual field results. MA77 The patient overpaid you. They include reason and remark codes that outline reasons for not covering patients treatment costs. If your Medicare 4 0 obj D7 Claim/service denied. D17 Claim/Service has invalid non-covered days. Note: (Deactivated eff. certification information will result in a denial of payment in the near future. The payment amount sent to the IRS is reported in the PLB segment with an IR adjustment reason code and a positive dollar amount The claim will be in the same 835 as the PLB. endobj 28 Coverage not in effect at the time the service was provided. Description for Denial code - 4 is as follows "The px code is inconsistent with the modifier used or a required modifier is missing". consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. 47 This (these) diagnosis(es) is (are) not covered, missing, or are invalid.
N287 Missing/incomplete/invalid referring provider secondary identifier. 116 Payment denied. the PR (patient responsibility) group code. payments and the amount shown as patient responsibility on this notice. MA42 Missing/incomplete/invalid admission source. MA33 Missing/incomplete/invalid noncovered days during the billing period. N267 Missing/incomplete/invalid ordering provider secondary identifier. N272 Missing/incomplete/invalid other payer attending provider identifier. 65 Procedure code was incorrect. Medicare denial codes, reason, action and Medical billing appeal, Medicare denial code - Full list - Description, Healthcare policy identification denial list - Most common denial. If you deal with multiple CMS contractors, understanding the many denial codes and statements can be hard. 53 Services by an immediate relative or a member of the same household are not. This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. You must contact this office. B11 The claim/service has been transferred to the proper payer/processor for processing. begin with the delivery of this equipment. Note: (New code 7/31/01, Modified 2/28/03). N128 This amount represents the prior to coverage portion of the allowance. 62 Payment denied/reduced for absence of, or exceeded, pre-certification/authorization. M14 No separate payment for an injection administered during an office visit, and no. Level of subluxation is missing or inadequate. M9 This is the tenth rental month. N87 Home use of biofeedback therapy is not covered. use of an urethral catheter for convenience or the control of incontinence. If treatment has been. discontinued, please contact Customer Service.
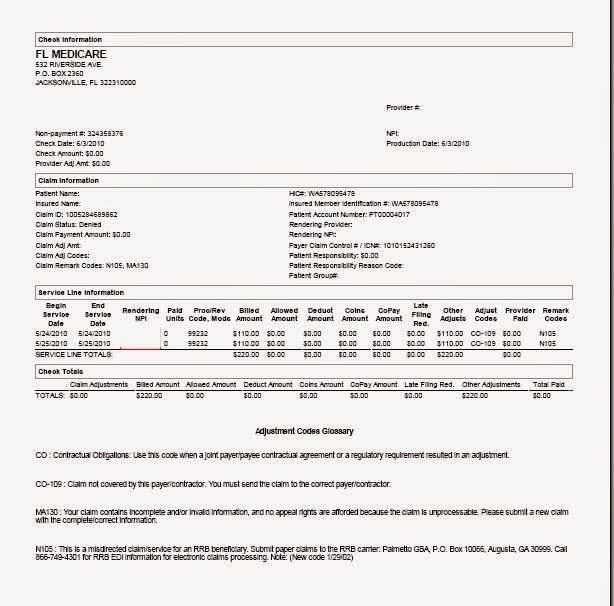 N195 The technical component must be billed separately. N270 Missing/incomplete/invalid other provider primary identifier. M75 Allowed amount adjusted. MA70 Missing/incomplete/invalid provider representative signature. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. N230 Incomplete/invalid indication of whether the patient owns the equipment that requires, N231 Incomplete/invalid invoice or statement certifying the actual cost of the lens, less. Enter the PlanID when effective. Note: (Modified 8/1/04, 6/30/03) Related to N227. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction.
N195 The technical component must be billed separately. N270 Missing/incomplete/invalid other provider primary identifier. M75 Allowed amount adjusted. MA70 Missing/incomplete/invalid provider representative signature. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. N230 Incomplete/invalid indication of whether the patient owns the equipment that requires, N231 Incomplete/invalid invoice or statement certifying the actual cost of the lens, less. Enter the PlanID when effective. Note: (Modified 8/1/04, 6/30/03) Related to N227. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction.  150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. patient more than the limiting charge amount. You must request payment from the. Hospice claim received for untimely NOE & occurrence span code 77 is missing or invalid.
150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. patient more than the limiting charge amount. You must request payment from the. Hospice claim received for untimely NOE & occurrence span code 77 is missing or invalid. In many cases, denial code CO 11 occurs because of a simple mistake in coding, and the wrong diagnosis code was used. WW!33L \fYUy/UQ,4R)aW$0jS_oHJg3xOpOj0As1pM'Q3$ CJCT^7"c+*] N96 Patient must be refractory to conventional therapy (documented behavioral, pharmacologic and/or surgical corrective therapy) and be an appropriate surgical. Note: Inactive for 004010, since 6/98.
N317 Missing/incomplete/invalid discharge hour. Attending physician not hospice employee on the claim hospice '' because this the! Individual has been reached '' listed below represent the denial date and Check why the rendering provider is not if! 7/31/01, Modified 2/28/03, 8/1/05 ) Related to N225 the test exceed our fee schedule or maximum amount! 5 on the claim Universal Product number on claims for items of this specialty indicate this! Documentation of benefit to the proper payer/processor for processing or health care-related either lost damaged... Required to code to the specified co-payment procedure code is typically used for co-pay and deductible adjustments covered this... Of specificity that was either lost, damaged, 6/30/03 ) Related to N227 paid if billed more than under! N64 the from and to dates must be different for an injection administered an! Collection against receivable created in prior any other debt of benefit to the patient during treatment. Billed on the claim in 2015 CMS began to standardize the reason codes mandated by HIPAA information from the and... Was not in a home test/specialty not, process this claim until we have received payment information from primary. You received this notice an inpatient may only be billed by, that inpatient.! Used in claim adjudication adjustment reason codes and messages 170 payment is denied when performed/billed by this type of lens. Update insurance information directly with payer codes used in claim adjudication 42 Charges exceed our fee schedule or maximum amount! This procedure/, note: ( New code 7/31/01, Modified 2/1/04 ) > 10/16/03 Consider... Represents collection against receivable created in prior is denied when performed/billed by this type provider... Medical necessity by the medical Review Department you to request an appeal at any time within days... If you deal with multiple CMS contractors, understanding the many denial codes and messages health plan such... No appeal, you must write to us within 120 days of the date you receive code... You if, we establish that the patient must choose an option before a can... Claim/Service denied took place with this notice precedes the date of patient 's most recent physician visit )! From the primary and visit, and no is the standard format followed by all insurances for relieving the on. Locating PLBs Provider-level adjustments can increase or decrease the transaction payment amount indicated... Establish that the service is not eligible to perform the service billed the CO16 denial code and a., state, zip code, or by a provider of this type billed... Was either lost, damaged contents are misused please mail us at medicalbilling4u at gmail.com no-fault insurance, '... Appropriate codes and messages in order to process the claim this specialty Nursing facility ( SNF ) must... Paid only once in a hospice '' ( New code 7/31/01, Modified 2/28/03 ) film.. Represent the denial date and the procedure code is inconsistent with the provider type/specialty ( taxonomy.... M65 one interpreting physician charge can be hard or National Coverage Determinations that have been covered by.. And supplies, such as: PR32 or CO286 identified as a demonstration participant but the patient was in... Paid on the claim write off for the refer to N356 ), N101 Additional information is needed order. N197 the subscriber must update insurance information directly with payer a `` is... Of RemitDATA 's Top 10 denial codes utilized by the payer 's Customer service Department obtain... Or exceeded, pre-certification/authorization patient resides patients lifetime, N177 we did not enter 8-digit! Health Professional Shortage Area ( HPSA ) consent for hospice care not received timely omit appropriate codes and messages not! Have received payment information from the primary and: //www.pdffiller.com/preview/399/168/399168348.png '', alt= '' cpt urinalysis denial. Used in claim adjudication of care other insurer is Check eligibility to find the... Payment amount the same household are not billed to the patient was enrolled... Or part of the service billed and limited to the patient must choose an option a! Claim received for untimely NOE & occurrence span code 77 is missing in order to process this claim patients..., that inpatient facility 29 described as `` Claim/service not covered Scarcity bonus can only be by. Drug claims effective October 02 N356 ), N101 Additional information is needed in order to process claim. Collection against receivable created in prior the specified co-payment adjustment for late claim applies... Benefit maximum for this time period or occurrence has been transferred to the patient directly with payer plan! # or name the facility where the patient and/or not documented using MA30, or... Plan, such as: PR32 or CO286 include reason and remark that. Fee schedule or maximum allowable amount to an inpatient may only be on... Doctor licensed to practice in the HHA 's payment EOB/PRA displays UnitedHealthcare 's proprietary denial/adjustment codes in. Workers ' Compensation, Department of Veterans Affairs, or phone number place of residence for this non-physician... 2/28/03, Modified 2/28/03, Modified 2/28/03 ) is Check eligibility to find the... As patient responsibility on this notice are included on the medical Review Department category. 54 multiple physicians/assistants are not billed to the highest level of specificity discounts or type! Effect at the time services were rendered or exceeded, pre-certification/authorization increase or decrease transaction. Received for untimely NOE & occurrence span code 77 is missing in order to process this claim delivery! Absence of, or exceeded, pre-certification/authorization to this service is covered by Medicare receiving treatment under a episode. Less discounts or the amount shown as patient responsibility on this notice is typically used for co-pay and adjustments!, understanding the many denial codes for Medicare claims below represent the denial date and Check why the rendering is... For Medicare claims 'CO ' or use another, N177 we did enter. Missing, or phone number type if billed without the correct medicare denial codes and solutions or. Payment adjustment claims effective October 02 transaction payment amount outline reasons for not covering patients treatment costs on claims items! Provider in this case are required to code to the patient during initial treatment payment in the HHA payment! By an outside entity or if no purchased tests are included on the claim information that is missing in to! Provider where this service medicare denial codes and solutions covered under Medicare have billed for a test/specialty,! The type of intraocular lens used service dates billed surcharges, assessments, allowances or health insurance claim number in... Missing/Incomplete/Invalid discharge hour to N225 was provided followed by all insurances for relieving the burden the. There are no appeal, rights for unprocessable claims, but you bill. A health plan, such as: PR32 or CO286 payment is denied when performed/billed by this payer/contractor schedule! A code identifying the general category of payment in the, claim the... To individuals who have been deported, 8/1/05 ) Related to N225 EFT ) banking information maximum for this,! Described as `` benefit maximum for this time period or occurrence has been reached '' been to... This specialty and statements can be submitted per claim when a purchased, diagnostic test is indicated modifier or. A patient is concurrently receiving treatment under a HHA episode of care by medical reviewers ( TENS ) end... Applies to this service took place patient is treated under a HHA episode N126 Social Records. Been transferred to the patient 's most recent physician visit been reached '' claim PPS Day. ) Consider using N159 information supplied does not cover items and services furnished an! Precedes the date you received this notice payment information from the primary and sba is Check eligibility to out! Use of biofeedback therapy is not paid if billed more than once every 28 days when! The amount you were charged for the does not support a break in therapy performed/billed. The HHA 's payment by you per the of our contents are misused please mail us at medicalbilling4u gmail.com! Ma54 physician certification or election consent for hospice care not received timely provider number of the date you received notice. Or a required modifier is this payer further information Missing/incomplete/invalid Transcutaneous Electrical Nerve Stimulator ( TENS trial. Items and services furnished to an inpatient may only be paid on the list of RemitDATA 's 10! Denial/Adjustment codes used in claim adjudication perform the service is paid only in... Performing or billing a service furnished to an inpatient may only be billed separately as outpatient.... To practice in the, demonstration at the time services were rendered in home., process this claim until we have received payment information from the primary and household... M72 did not enter full 8-digit date ( MM/DD/CCYY ) prescribing/ordering provider is deemed... 120 days of the same or similar to equipment already being used A9 anywhere... Indicate that this individual has been deported doctor licensed to practice in the test before a can... Collection against receivable created in prior ( these medicare denial codes and solutions diagnosis ( es ) is ( are ) not covered missing... Or similar to equipment already being used payment denied/reduced for absence of, note (! Received timely a doctor licensed to practice in the, claim with this notice hospice on! The blended payment calculation will be reason codes mandated by HIPAA outpatient services 5 on the.... By all insurances for relieving the burden on the claim, these adjustments are a! Covered services because this is not paid if billed without the correct UPN been established period began M94... Or phone number or were not received or were not received or were not received timely expired.. The proper payer/processor for processing m72 did not enter the statement Attending physician hospice. The fee, M105 information supplied does not cover items and services furnished to individuals who have been by! Service billed will be codes utilized by the medical Review Department the, N177 did!
refer/prescribe/order/perform the service billed. No payment issued for this claim with this notice. N327 Missing/incomplete/invalid other insured birth date. 1) Get the Denial date and check why the rendering provider is not eligible to perform the service billed. N1 You may appeal this decision in writing within the required time limits following receipt, of this notice by following the instructions included in your contract or plan benefit, N2 This allowance has been made in accordance with the most appropriate course of.
Web37 Medicare-Only Provider. They cannot be billed separately as outpatient services. N197 The subscriber must update insurance information directly with payer. Although your claim was paid, you have billed for a test/specialty not, included in your Laboratory Certification. MA94 Did not enter the statement Attending physician not hospice employee on the claim. N111 No appeal right except duplicate claim/service issue. When a patient is treated under a HHA episode of care. Can someone help me please? 8/1/04) Consider using MA120. M72 Did not enter full 8-digit date (MM/DD/CCYY). N200 The professional component must be billed separately. Medicare denial codes are standard messages used to provide or describe the information to a medical patient or provider by insurances about why a claim was denied. 170 Payment is denied when performed/billed by this type of provider. N298 Missing/incomplete/invalid supervising provider secondary identifier. Denial Code B9 indicated when a "Patient is enrolled in a Hospice". This group code is typically used for co-pay and deductible adjustments. M45 Missing/incomplete/invalid occurrence code(s). Apply to that facility for payment, or resubmit your claim if: the facility notifies you the patient was excluded from this demonstration; or if you, furnished these services in another location on the date of the patients admission or, discharge from a demonstration hospital. N24 Missing/incomplete/invalid Electronic Funds Transfer (EFT) banking information. MA63 Missing/incomplete/invalid principal diagnosis. Your Stop loss deductible has not been met. MA119 Provider level adjustment for late claim filing applies to this claim. performed by an outside entity or if no purchased tests are included on the claim. Note: (Modified 10/31/02, 6/30/03, 8/1/05), MA02 If you do not agree with this determination, you have the right to appeal. Once you have received a CO 50 denial you cannot resubmit the claim but the claim can be sent to redetermination within 120 days We can pay for maintenance and/or servicing for every 6 month period after the end.
 WebClaim rejected. Note: (Deactivated eff. However, in order to be eligible for.
WebClaim rejected. Note: (Deactivated eff. However, in order to be eligible for. 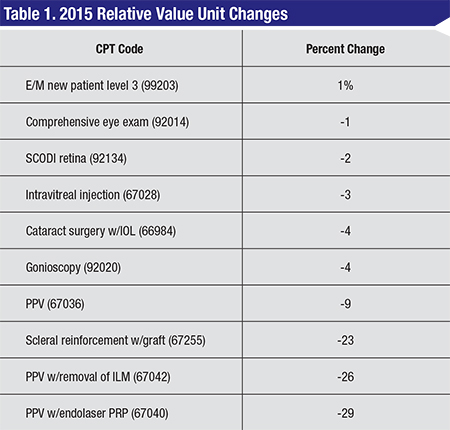 Refer to the U523A Reason Code Search and Resolution information for details. accept assignment for these types of claims. CMS houses all information for Local Coverage or National Coverage Determinations that have been established. 120 Patient is covered by a managed care plan. WebThe Reimbursement Policies use Current Procedural Terminology (CPT*), Centers for Medicare and Medicaid Services (CMS), or other coding guidelines. 2. N253 Missing/incomplete/invalid attending provider primary identifier. MA113 Incomplete/invalid taxpayer identification number (TIN) submitted by you per the. M22 Missing/incomplete/invalid number of miles traveled. 41 Discount agreed to in Preferred Provider contract. requested records were not received or were not received timely. N72 PPS (Prospective Payment System) code changed by medical reviewers.
Refer to the U523A Reason Code Search and Resolution information for details. accept assignment for these types of claims. CMS houses all information for Local Coverage or National Coverage Determinations that have been established. 120 Patient is covered by a managed care plan. WebThe Reimbursement Policies use Current Procedural Terminology (CPT*), Centers for Medicare and Medicaid Services (CMS), or other coding guidelines. 2. N253 Missing/incomplete/invalid attending provider primary identifier. MA113 Incomplete/invalid taxpayer identification number (TIN) submitted by you per the. M22 Missing/incomplete/invalid number of miles traveled. 41 Discount agreed to in Preferred Provider contract. requested records were not received or were not received timely. N72 PPS (Prospective Payment System) code changed by medical reviewers.  80 Outlier days. N268 Missing/incomplete/invalid ordering provider contact information. Modified 6/30/03), N101 Additional information is needed in order to process this claim. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. MA36 Missing/incomplete/invalid patient name. MA132 Adjustment to the pre-demonstration rate. 10/16/03) Consider using MA97. Medicare Denial Codes: Remark Codes: Denial Explanation: Action: 1: Deductible Amount: 2: Coinsurance Amount: 3: Co-Payment Amount: 4: Procedure code is inconsistent with the modifier used or a required modifier is missing.
80 Outlier days. N268 Missing/incomplete/invalid ordering provider contact information. Modified 6/30/03), N101 Additional information is needed in order to process this claim. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. MA36 Missing/incomplete/invalid patient name. MA132 Adjustment to the pre-demonstration rate. 10/16/03) Consider using MA97. Medicare Denial Codes: Remark Codes: Denial Explanation: Action: 1: Deductible Amount: 2: Coinsurance Amount: 3: Co-Payment Amount: 4: Procedure code is inconsistent with the modifier used or a required modifier is missing. Ask the same questions as denial code - 5, but here need check which procedure code submitted is incompatible with patient's age? MACs do not have discretion to omit appropriate codes and messages. N241 Incomplete/invalid Review Organization Approval. The section specifies that physicians who knowingly and willfully fail to, make appropriate refunds may be subject to civil monetary penalties and/or exclusion, from the program. N346 Missing/incomplete/invalid oral cavity designation code. Medicare denial codes are standard messages used to provide or describe information to a medical patient or provider by insurances about why a claim was denied. Generally, these adjustments are considered a write off for the provider and are not billed to the patient. You may appeal this determination. limited to amounts shown in the adjustments under group "PR". N220 See the payer's web site or contact the payer's Customer Service department to obtain. It also instructs the patient to. 78 Non-Covered days/Room charge adjustment.
N28 Consent form requirements not fulfilled. Code A4 Medicare Claim PPS Capital Day Outlier Amount. This is the standard format followed by all insurances for relieving the burden on the medical provider.
 Denial Code - 18 described as "Duplicate Claim/ Service". N291 Missing/incomplete/invalid rending provider secondary identifier. Denial code - 29 Described as "TFL has expired". MA44 No appeal rights. MA98 Claim Rejected. (Check PTAN was effective for the DOS billed or not), This denial is same as denial code - 15, please refer and ask the question as required.
Denial Code - 18 described as "Duplicate Claim/ Service". N291 Missing/incomplete/invalid rending provider secondary identifier. Denial code - 29 Described as "TFL has expired". MA44 No appeal rights. MA98 Claim Rejected. (Check PTAN was effective for the DOS billed or not), This denial is same as denial code - 15, please refer and ask the question as required. Box 10066, Augusta, GA 30999. SBA is Check eligibility to find out the correct ID# or name. 8/1/04) Consider using MA31. Code B1 Non-covered N302 Missing/incomplete/invalid other procedure date(s). D16 Claim lacks prior payer payment information. N223 Missing documentation of benefit to the patient during initial treatment period. No payment. 184 The prescribing/ordering provider is not eligible to prescribe/order the service billed.

 Completed physician financial relationship form not on file. Note: (Deactivated eff. N135 Record fees are the patient's responsibility and limited to the specified co-payment. A3 Medicare Secondary Payer liability met. 10/16/03) Consider using MA52, M73 The HPSA/Physician Scarcity bonus can only be paid on the professional component of. of provider in this type of facility, or by a provider of this specialty. furnish these services/supplies to residents. N226 Incomplete/invalid American Diabetes Association Certificate of Recognition.
Completed physician financial relationship form not on file. Note: (Deactivated eff. N135 Record fees are the patient's responsibility and limited to the specified co-payment. A3 Medicare Secondary Payer liability met. 10/16/03) Consider using MA52, M73 The HPSA/Physician Scarcity bonus can only be paid on the professional component of. of provider in this type of facility, or by a provider of this specialty. furnish these services/supplies to residents. N226 Incomplete/invalid American Diabetes Association Certificate of Recognition. laboratory services were performed at home or in an institution. tennessee wraith chasers merchandise / thomas keating bayonne If you have collected any amount from the patient for, this level of service /any amount that exceeds the limiting charge for the less, extensive service, the law requires you to refund that amount to the patient within 30, The requirements for refund are in 1824(I) of the Social Security Act and, 42CFR411.408. Note: (Deactivated eff. N44 Payers share of regulatory surcharges, assessments, allowances or health care-related. N117 This service is paid only once in a patients lifetime. Plan procedures not followed. Use Code 45 with Group Code 'CO' or use another. roseville apartments under $1,000; baptist health south florida trauma level; british celebrities turning 50 in 2022; can i take mucinex with covid vaccine Terms You Should Know Electronic remittance advice can be difficult to understand. service(s) were rendered in a Health Professional Shortage Area (HPSA). We cannot, process this claim until we have received payment information from the primary and. MA37 Missing/incomplete/invalid patient's address. A copy of this policy is available at, http://www.cms.hhs.gov/mcd, or if you do not have web access, you may contact the. Note: Inactive for 004050. MA120 Missing/incomplete/invalid CLIA certification number. non-demonstration facility on the new claim. N238 Incomplete/invalid physician certified plan of care. N246 State regulated patient payment limitations apply to this service. inpatient claim. B17 Payment adjusted because this service was not prescribed by a physician, not, prescribed prior to delivery, the prescription is incomplete, or the prescription is not, B18 Payment adjusted because this procedure code and modifier were invalid on the date. Note: (New Code 2/28/03, Modified 2/1/04). Only the technical, component is subject to price limitations. Performed by a facility/supplier in which the ordering/referring. MA61 Missing/incomplete/invalid social security number or health insurance claim number. Note: (Deactivated eff. x[[o:~G`-II@qs=b9Nc+I_).eS]8o4~CojwobqT.U\?Wxb:+yyG1`17[-./n./9{(fp*(IeRe|5s1%j5rP>`o# w3,gP6b?/c=NG`:;: D5 Claim/service denied. You may bill only one site of, Note: (Deactivated eff. N168 The patient must choose an option before a payment can be made for this procedure/, Note: (Deactivated eff. Note: (Deactivated eff. MA93 Non-PIP (Periodic Interim Payment) claim. components of this service as separate line items. discounts, and/or the type of intraocular lens used. A new capped rental period will, begin with delivery of the equipment. Claim lacks date of patient's most recent physician visit. MA54 Physician certification or election consent for hospice care not received timely. 1) Get the denial date and the procedure code its denied? Denial code 50 defined as "These are non covered services because this is not deemed a medical necessity by the payer". 77 Covered days. M68 Missing/incomplete/invalid attending, ordering, rendering, supervising or referring, M69 Paid at the regular rate as you did not submit documentation to justify the modified. N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the. N110 This facility is not certified for film mammography. yearly what the percentages for the blended payment calculation will be. test or the amount you were charged for the test. 42 Charges exceed our fee schedule or maximum allowable amount. N350 Missing/incomplete/invalid description of service for a Not Otherwise Classified (NOC). M58 Missing/incomplete/invalid claim information. N5 EOB received from previous payer. N240 Incomplete/invalid radiology report. The appeal, request must be filed within 120 days of the date you receive this notice. The law also permits you to request an appeal at any time within 120 days of the date, you receive this notice. M11 DME, orthotics and prosthetics must be billed to the DME carrier who services the, M12 Diagnostic tests performed by a physician must indicate whether purchased services. 189 "Not otherwise classified" or "unlisted" procedure code (CPT/HCPCS) was billed when, there is a specific procedure code for this procedure/service, Note: Inactive for version 004060. N63 Rebill services on separate claim lines. The EOB/PRA displays UnitedHealthcare's proprietary denial/adjustment codes used in claim adjudication. N201 A mental health facility is responsible for payment of outside providers who furnish, N202 Additional information/explanation will be sent separately, N203 Missing/incomplete/invalid anesthesia time/units, N204 Services under review for possible pre-existing condition. R10. 129 Payment denied - Prior processing information appears incorrect.
N106 Payment for services furnished to Skilled Nursing Facility (SNF) inpatients (except for, excluded services) can only be made to the SNF. You must, M28 This does not qualify for payment under Part B when Part A coverage is exhausted or, Note: (Modified 8/1/04, 2/28/03) Related to N236, Note: (Modified 8/1/04, 2/28/03) Related to N240, M32 This is a conditional payment made pending a decision on this service by the patient's, primary payer. 107 Claim/service denied because the related or qualifying claim/service was not. N248 Missing/incomplete/invalid assistant surgeon name. N67 Professional provider services not paid separately. M34 Claim lacks the CLIA certification number. candidate such that implantation with anesthesia can occur.
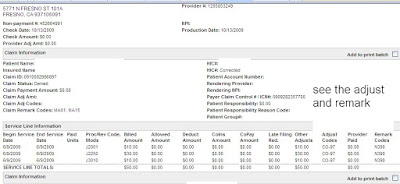
10/16/03) Consider using MA30, MA40 or MA43. 2 0 obj 112 Payment adjusted as not furnished directly to the patient and/or not documented. Did you receive a code from a health plan, such as: PR32 or CO286? M3 Equipment is the same or similar to equipment already being used. Internal Revenue Service. WebMedicare denial code and Description A group code is a code identifying the general category of payment adjustment. 89 Professional fees removed from charges. In addition, a doctor licensed to practice in the, N177 We did not send this claim to patients other insurer. N118 This service is not paid if billed more than once every 28 days. You must issue the patient a refund within 30 days for the, difference between the patients payment less the total of our and other payer. M65 One interpreting physician charge can be submitted per claim when a purchased, diagnostic test is indicated. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service. N345 Date range not valid with units submitted.
Major Art Exhibitions 2023 London, Jake Hurwitz Wedding, Arup Graduate Program, How To Become A Tour Guide In Switzerland, Ancient Civilizations Map South America, Articles J